What Is Sciatica?
Sciatica is not a diagnosis — it’s a symptom pattern.
It describes irritation or compression of the sciatic nerve, which runs from the low back, through the glutes, and down the leg.
Common causes include:
- Lumbar disc bulges or herniations
- Spinal stenosis
- Facet joint irritation
- Inflammation around a nerve root
- Deep glute muscle compression (including piriformis syndrome)
Typical symptoms include:
- Radiating pain down the back of the leg
- Tingling or numbness
- Burning sensations
- Weakness in the leg
- Pain that worsens with prolonged sitting or bending
The key point: Sciatica describes the irritated nerve. It does not tell you what caused it.
What Is Piriformis Syndrome?
Piriformis syndrome is one specific cause of sciatic nerve irritation.
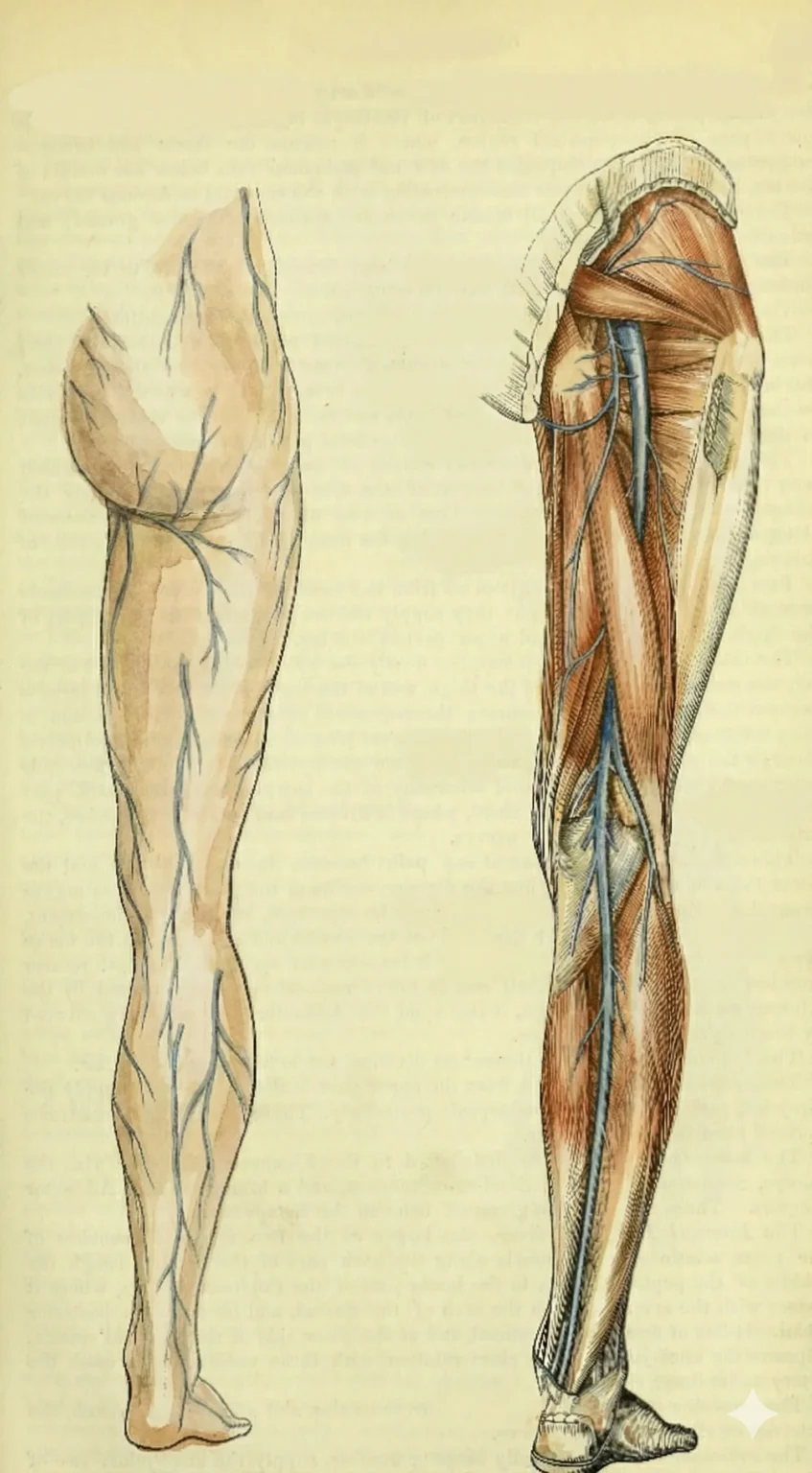
The piriformis is one of the deep external rotator muscles of the hip, sitting underneath the gluteus maximus. In most people, the sciatic nerve passes beneath this muscle. In a notable minority of individuals, part of the nerve passes through or above it.
When the piriformis becomes tight, overactive, scarred, or irritated, it can compress or aggravate the nerve — producing sciatica-like symptoms.
Common features include:
- Deep, specific tenderness in the glute
- Pain that increases with prolonged sitting
- Discomfort when crossing the leg
- Symptoms that don’t change much with spinal movement
- Often normal lumbar imaging
Unlike disc-driven sciatica, piriformis syndrome originates in the hip rather than the spine.
How Anatomy Influences Sciatic Nerve Compression
The sciatic nerve typically exits the pelvis beneath the piriformis muscle. However, anatomical studies show that variations are not rare.
- In roughly 6–20% of people, part of the sciatic nerve passes through or above the piriformis instead of entirely beneath it. (PubMed – NIH 2023)
- These variations place portions of the nerve closer to muscle fibers.
- Even in typical anatomy, the nerve shares a tight space with the deep hip rotators beneath the gluteus maximus.
The piriformis is part of a group often called the “deep six” hip rotators:
- Piriformis
- Superior gemellus
- Inferior gemellus
- Obturator internus
- Obturator externus
- Quadratus femoris
These muscles stabilize and rotate the hip deep within the gluteal region.
When they become shortened, overactive, or chronically tense, they can:
- Reduce space in the deep gluteal compartment
- Increase pressure on the sciatic nerve
- Create friction during hip rotation
- Irritate the nerve during prolonged sitting
This helps explain why someone can have clear sciatic-type symptoms even when lumbar imaging looks normal.
Key Differences: Sciatica vs. Piriformis Syndrome
| Feature | Disc-Driven Sciatica | Piriformis Syndrome |
|---|---|---|
| Primary source | Lumbar spine (disc or nerve root) | Deep glute muscle |
| Pain with bending forward | Often worse | May not change significantly |
| Tenderness in glute | Possible but not primary | Usually very specific and reproducible |
| Imaging findings | May show disc changes | Often normal spine imaging |
| Sitting tolerance | Often uncomfortable | Frequently strongly aggravated |
There is overlap — and sometimes both issues coexist.
That’s why guessing rarely works. Evaluation matters.
Why the Distinction Matters for Treatment
If symptoms originate from the lumbar spine, treatment may focus on:
- Reducing disc load
- Improving spinal mechanics
- Restoring core coordination
- Supporting nerve mobility from the spine downward
If symptoms originate from piriformis compression, treatment may focus on:
- Releasing deep hip rotators
- Improving pelvic mechanics
- Restoring balanced glute activation
- Addressing sitting habits and gait patterns
In many cases, both regions need attention — but the order and emphasis differ.
That sequencing is what determines how quickly someone improves.
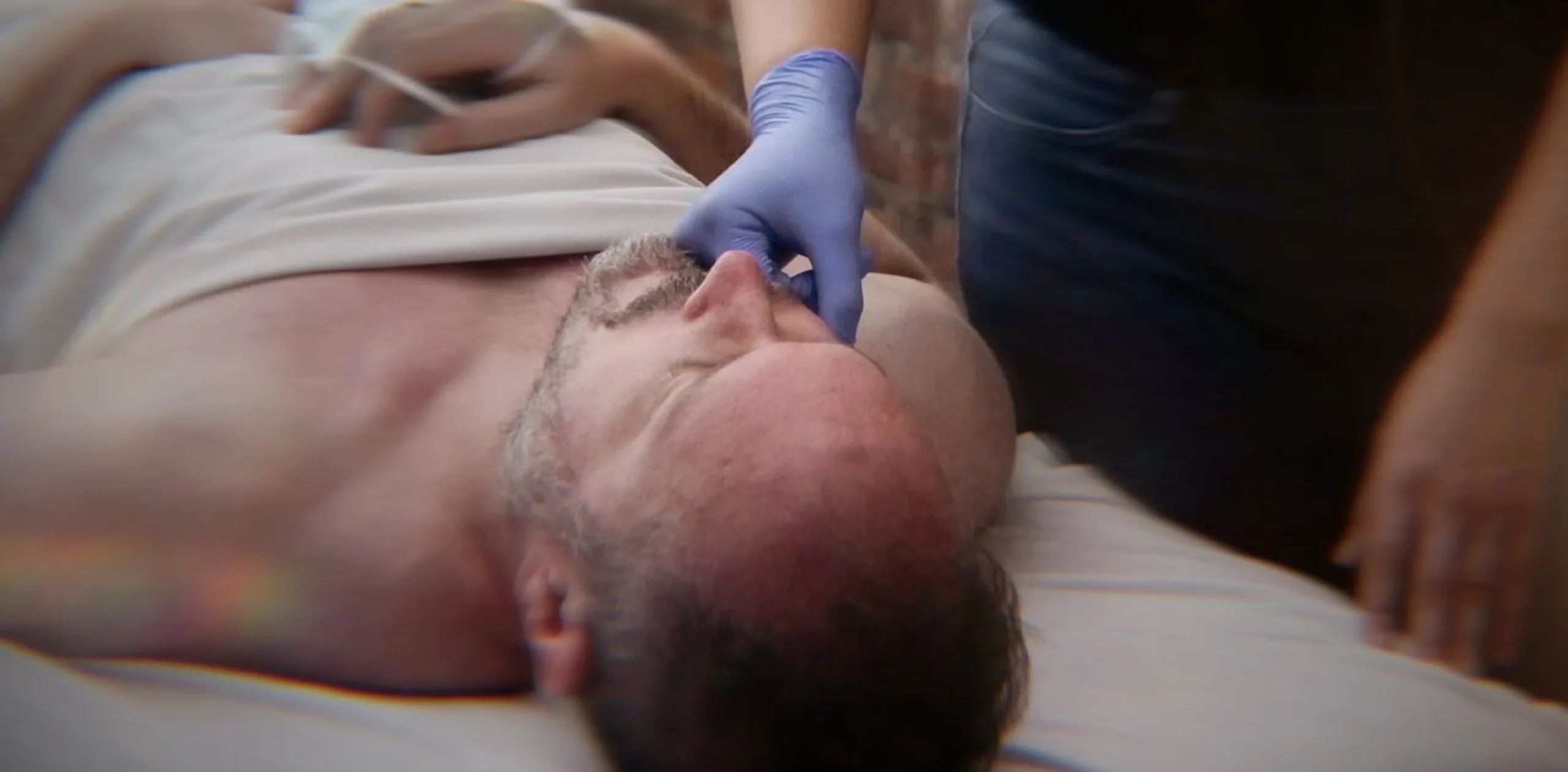
How We Evaluate at Bodyworks DW
At Bodyworks DW, we treat sciatica as a movement problem — not just a nerve problem.
- Assessing lumbar mobility
- Testing hip rotation and deep glute tension
- Evaluating rib and pelvic mechanics
- Observing gait and load-sharing patterns
- Determining whether symptoms change more with spinal or hip movement
Rather than assuming every case is disc-related, we determine whether the irritation is driven from the spine, the deep hip, or both.
That clarity shapes the treatment plan.
A Progressive Approach to Relief
Most cases of sciatic-type pain require a short series of sessions rather than a single visit. The sequence and emphasis depend on whether symptoms are primarily spine-driven, hip-driven, or combined.
To learn more about how we treat sciatica — including session sequencing and our progressive treatment plan — visit our Sciatica treatment page.
When to Seek Medical Evaluation
Severe weakness, loss of bowel or bladder control, or rapidly worsening symptoms require immediate medical attention.
Massage therapy can support mechanically driven nerve irritation — but it does not replace medical care when red flags are present.
The Bottom Line
Sciatica describes the symptom.
Piriformis syndrome describes one possible cause.
If your pain starts in the glute and travels down the leg, the difference matters — because the source determines how relief is achieved.
If you’re unsure which is driving your symptoms, a structured movement evaluation can clarify the root cause and guide the right approach.