Jaw Tension Is Increasing — and It’s Not Just “Stress”
Jaw tension is commonly caused by habitual clenching, stress-related muscle bracing, and forward head posture that overloads the jaw and neck. Short-term relief may come from heat and jaw awareness, but persistent tension often improves when TMJ motion, neck posture, and breathing mechanics are addressed together.
For many people, this pattern develops gradually. Teeth clenching and grinding often start as subtle responses to stress, long workdays, and poor posture. Over time, constant nervous system activation keeps the jaw muscles braced—even during sleep—leading to headaches, neck pain, and facial discomfort.
At first, the tension is subtle. Over time, it becomes automatic—during the day, at night, and often during sleep. Many people don’t realize they’re clenching until pain shows up elsewhere.
Left unaddressed, jaw tension can contribute to:
-
Clicking, popping, or locking in the jaw
-
Teeth sensitivity or damage from grinding
This isn’t just a jaw issue. It’s a whole-body pattern.
Why Jaw Tension Is Rarely Just About the Jaw
The temporomandibular joint (TMJ) sits in close relationship to the upper cervical spine. Tension in one almost always affects the other. Forward head posture (“text neck”), rib cage stiffness, uneven shoulder loading, and breathing mechanics all change how much work the jaw muscles are forced to do.
That’s why generic jaw massage or relaxation-focused bodywork often provides only short-term relief.
Effective care starts by asking better questions:
-
Is the tension one-sided?
-
Is one jaw joint working harder than the other?
-
Is neck position pulling the jaw forward?
-
Is stress showing up as bracing instead of movement?
When those factors aren’t addressed, the jaw keeps compensating—and the tension returns.
How Massage Therapy Helps Jaw Tension (When Done Correctly)
Targeted massage therapy can be very effective for jaw tension when it’s applied with precision and context.
That means:
-
Looking at posture and movement patterns, not just symptoms
-
Reducing tension in the neck, upper ribs, and shoulders to unload the jaw
-
Working with the primary chewing muscles, including the masseter
-
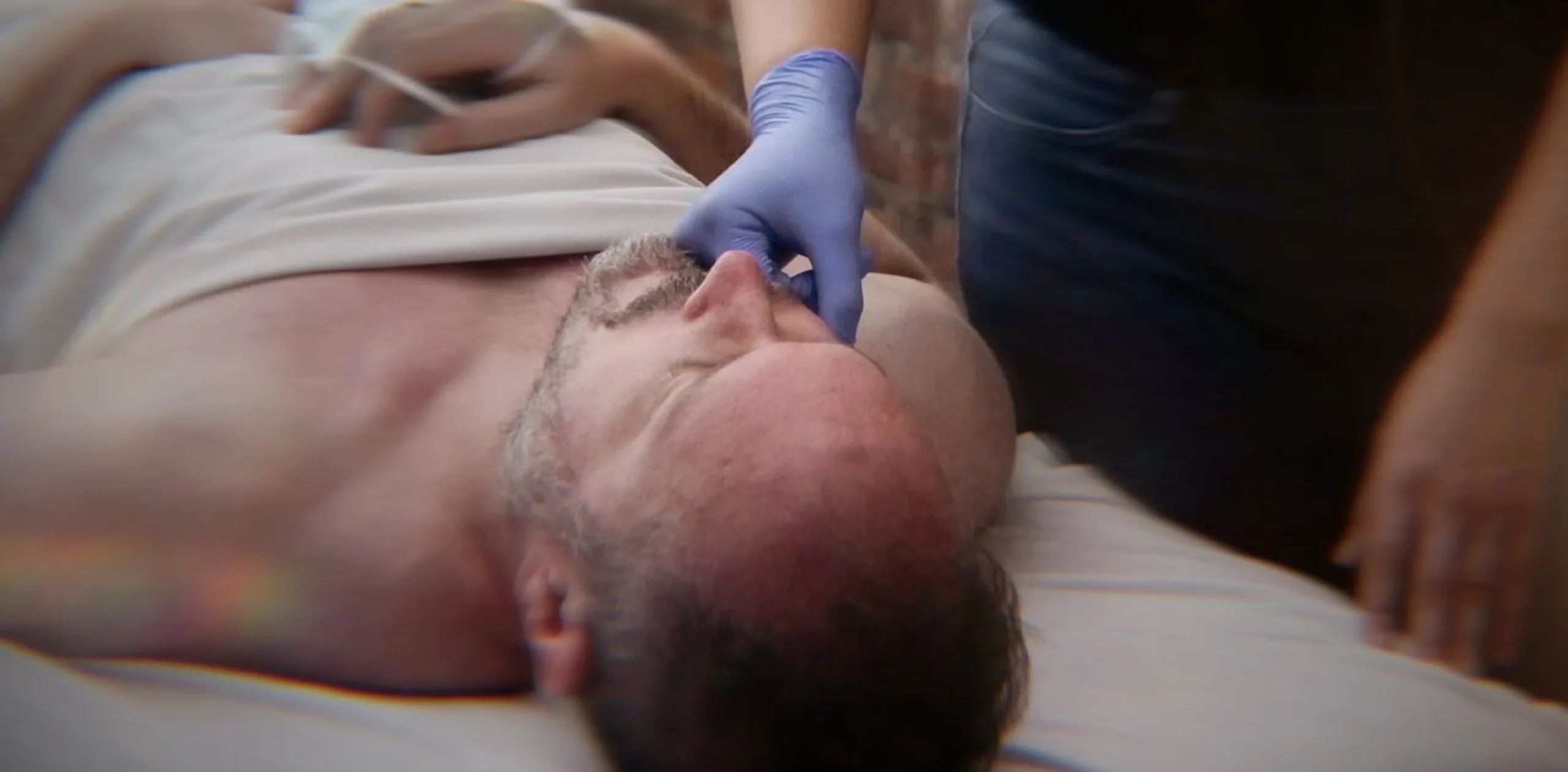
When appropriate, addressing deeper jaw muscles that can only be accessed intra-orally
Intra-oral (inner-mouth) work allows access to muscles like the pterygoids, which are heavily involved in clenching and grinding. These muscles are often overlooked and can be a key factor when jaw tension feels “stuck.”
This work is always done with clear communication, consent, and appropriate technique. While it can feel intense, clients often report:
-
Improved jaw range of motion
-
Reduced headache frequency
-
Less neck and upper shoulder tension
-
A noticeable sense of release through the face and throat
Not every headache or jaw issue is TMJ-related—but when jaw tension is the driver, targeted work can make a meaningful difference.
When It’s Time to Get Professional Help
Jaw tension is worth addressing professionally if it is:
-
Persistent or worsening
-
Accompanied by headaches or neck pain
-
Affecting sleep or daily comfort
-
Connected to clenching or grinding
Learn more about our TMJ & Jaw Pain Massage approach here
(Conservative, results-focused care that looks at how the jaw fits into the rest of the body.)
What You Can Do Between Sessions (Short-Term Support)
Between treatments, some people find temporary relief from:
-
Becoming aware of daytime clenching habits
-
Gentle heat applied to the jaw and upper neck
-
Slow nasal breathing to downshift nervous system tone
-
Light self-massage or tools like Gua Sha (used gently, not aggressively)
These strategies can help reduce load on the jaw and neck (see Neck Pain), but they don’t replace skilled, specific care when deeper patterns are involved.
Clinical Perspective: Treating Jaw Tension in Practice
Below is an earlier clinical discussion that offers additional insight into how jaw tension commonly presents and how it’s addressed in hands-on work.
Interview: Jaw Pain & TMJ — A Therapist’s Perspective
Elizabeth Dashiell interviews Senior Massage Therapist Laura Sniper
Elizabeth: What kind of pain do you most commonly address related to jaw tension?
Laura Sniper: One of the most common issues I treat—and one I really enjoy working with—is jaw pain. Many people don’t realize how much tension they’re holding there until we start working. The changes can be very noticeable for clients.
We also see a lot of neck pain. Neck tension often feeds directly into jaw tension. Over time, that can lead to habitual clenching during the day and at night. When jaw tension is ignored long-term, it may contribute to TMJ dysfunction.
Elizabeth: What exactly is TMJ disorder?
Laura Sniper: TMJ disorder involves the temporomandibular joint, which allows the jaw to move and open. Because it sits so close to the upper cervical spine, tension in the neck and jaw are closely linked.
When someone comes in with this kind of discomfort, I first look at posture—forward head position, asymmetries, and whether the pain is one-sided. Then I address those imbalances before doing local jaw work.
Elizabeth: What does the hands-on work involve?
Laura Sniper: I always work locally as well. That often includes the masseter muscle, which you can feel when you clench your jaw. In some cases, I also do intra-oral work to address deeper muscles like the pterygoids. These muscles are heavily involved in clenching and are commonly overlooked.
The work can feel intense, but many clients report improved jaw movement, less neck tension, and fewer headaches afterward—when jaw tension is the primary driver.
Common Questions About Jaw Tension
Why do I get jaw tension?
Jaw tension commonly comes from habitual clenching, stress, and forward head posture.
Can jaw tension cause headaches?
Yes — tension in jaw muscles often refers pain into the neck and head.
Is jaw tension the same as TMJ?
Jaw tension can be a part of TMJ dysfunction, but not all jaw tension is TMJ.